Our Group organises 3000+ Global Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ şÚÁĎÍř Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
şÚÁĎÍř Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
Indexed In
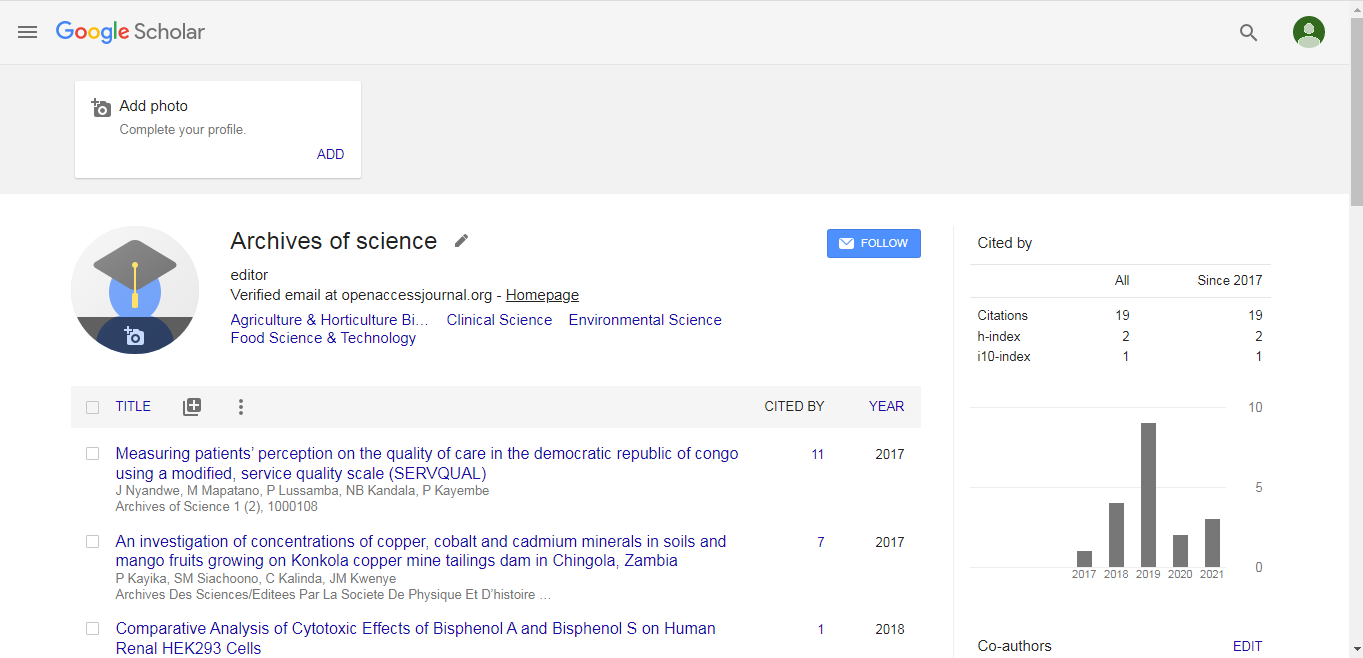
- Google Scholar
- ICMJE
Useful Links
Share This Page
Bridget Elizabeth Bax

Bridget Elizabeth Bax
Deputy Head
Molecular & Clinical Sciences Research Institute
Cell Biology and Genetics Research Centre
St. George’s University of London
London
E-mail: bebax@sgul.ac.uk
Biography
Diagnosis delays, lack of comprehension of disease pathophysiology, poor co-ordination of care and no approved therapies are the challenges that face a majority of the rare disease community. Over 7,000 rare diseases have been identified, but to date there are only around 400 licenced treatments on the market, creating a huge unmet need. Dr Bax’s research focuses on two objectives: i) to improve the understanding of the underlying pathogenic molecular mechanisms of rare inherited diseases and ii) to develop cell-based therapies for diseases with unmet needs. Currently her team are focusing on the fatal, ultra-rare disease, mitochondrial neurogastrointestinal encephalomyopathy (MNGIE).
Research Interest
To advance the understanding of the pathophysiological mechanisms and metabolic derangements that contribute to the complex phenotype exhibited in MNGIE, Dr Bax’s team are employing a range of proteomic and genomic technologies for the identification and validation of biomarkers in patient samples and in vitro models of MNGIE. The goals of this work are to provide a means of monitoring more effectively clinical and biochemical response to therapy (see below), to enable the tracking of disease progression in diagnosed patients, and to identify potentials targets for therapeutic intervention. With regard to cell based therapy development, Dr Bax has 20 years of experience in developing the autologous erythrocyte as a vehicle for delivering enzyme replacement therapies and other therapeutic proteins. The encapsulation technology has the advantage of prolonging the circulatory half-life of proteins, minimizing immunogenic reactions and negating the need for expensive chemical modification. She translated this therapeutic approach into the clinical setting through the development of enzyme replacement therapies for the compassionate treatment of adenosine deaminase deficiency and mitochondrial neurogastrointestinal encephalomyopathy due to thymidine phosphorylase deficiency. For 13 years she managed a contract with the Hampshire Primary Care Trust on behalf of the South of England Specialised Commissioning group for the treatment of an adult patient with adenosine deaminase deficiency. Erythrocyte encapsulated thymidine phosphorylase (EE-TP) is currently under clinical development for the treatment of MNGIE and a European clinical trial jointly funded by the MRC and Orphan Technologies is due to commence later in 2017. Orphan Drug Designation for EE-TP has been granted by both the Food and Drug Administration (USA) and European Medicines Agency.