Pn1 Involvement Independently Affects Long-Term Survival of Pn2 StageNon-Small Cell Lung Cancer after Thoracic Surgery
*Corresponding Author: Georg Schlachtenberger, Department of Cardiothoracic Surgery, University Clinic of Cologne, Kerpenerstrasse, Cologne, Germany, Tel: +49 22132722, Email: Schlachtenberger@uk-koeln.deReceived Date: Apr 01, 2021 / Accepted Date: Apr 15, 2021 / Published Date: Jun 22, 2021
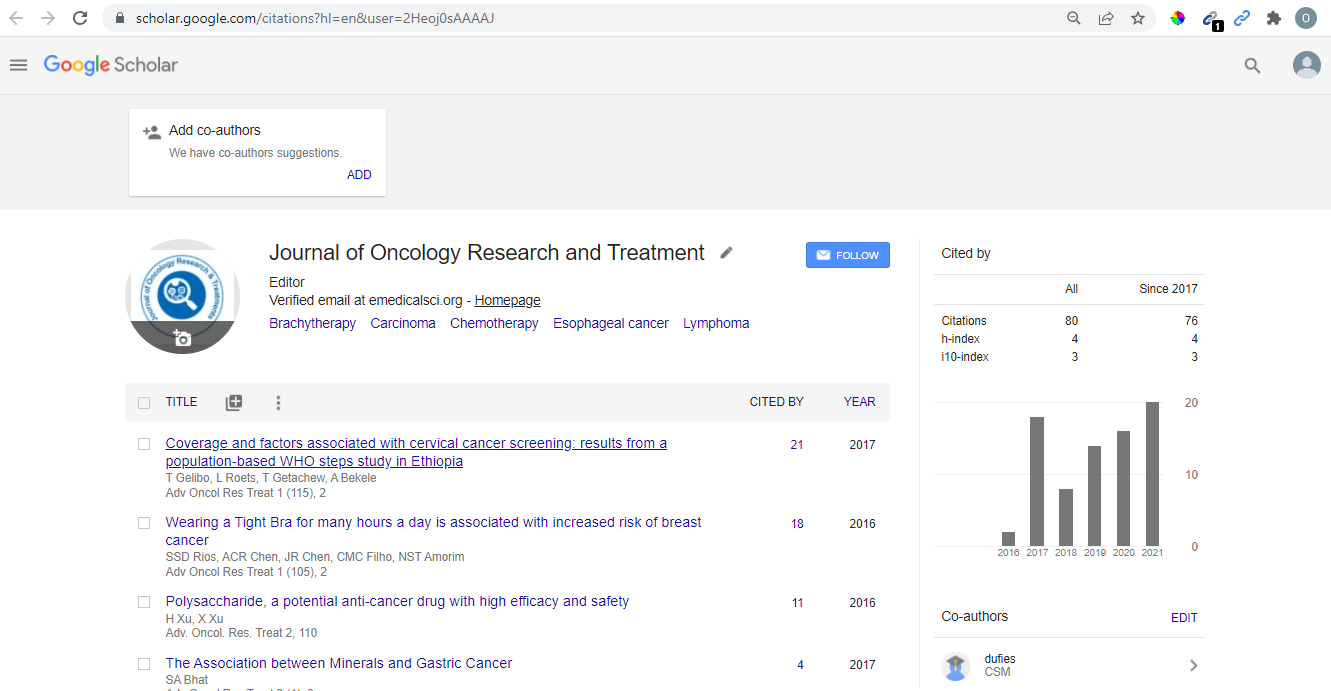
Citation: Schlachtenberger G, Doerr F, Menghesha H, Heldwein MB, Michel M, et al. (2021) Pn1 Involvement Independently Affects Long-Term Survival of Pn2 Stage Non-Small Cell Lung Cancer after Thoracic Surgery. J Oncol Res Treat S1:004.
Copyright: © 2021 Schlachtenberger G, et al. This is an open -access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Lung cancer remains the most common cause of cancer death worldwide. Anatomical lung resection remains the standard in early-stage lung cancer, but the ideal therapy for advance-stage Non-Small Cell Lung Cancer (NSCLC) with pN2 lymph node involvement remains controversial. In most cases pN1 and pN2 lymph nodes are affected consecutively (N1N2). Nevertheless, pN2 metastases also occur without pN1 involvement-termed skip-N2 metastases (N0N2). We reviewed current literature regarding the overall survival of N0N2. Furthermore, we discussed the possibilities of implementing N0N2 into the guidelines and if those patients would benefit from a different treatment modality.
Summary: According to the literature, N0N2 is a prognostic factor for long-term survival in pN2 stage patients compared to N1N2. The overall survival of N0N2 patients is similar to pN1 stage NSCLC patients. Despite significant long-term survival differences, the current guidelines do not distinguish between N0N2 and N1N2. In our opinion, patients with N0N2 and N1N2 should receive different therapies. It would be beneficial to evaluate the pN1 involvement preoperatively, in order to provide different therapeutic approaches for N0N2 and N1N2 patients. However, such a strategy is dependent on the efficiency of intrapulmonary lymph node assessment.
Key messages: N0N2 patients show significantly higher survival rates compared to patients with N1N2. Overall, pN2-stage NSCLC patients would benefit from a more sophisticated preoperative intrapulmonary lymph node assessment allowing for a more precise multimodal therapy.