Research Article
Time-Dependent Compensatory Responses to Chronic Neuroinflammation in Hippocampus and Brainstem: The Potential Role of Glutamate Neurotransmission
Holly M Brothers1, Isabelle Bardou1, Sarah C Hopp3, Yannick Marchalant2, Roxanne M Kaercher1, Sarah M Turner1, Mollie R Mitchem1, Kristina Kigerl3 and Gary L Wenk1*
1Department of Psychology, Ohio State University, Columbus, OH, USA
2NICN, UMR 6184, Universite de la Maditerranee, Marseille, France
3Department of Neuroscience, Ohio State University, Columbus, OH, USA
- Corresponding Author:
- Gary L Wenk
Department of Psychology
Ohio State University, Columbus
Ohio, USA, 43210
Tel: 614-688-3404
Fax: 614-688-4733
E-mail: wenk.6@osu.edu
Received date: February 27, 2013; Accepted date: March 21, 2013; Published date: March 28, 2013
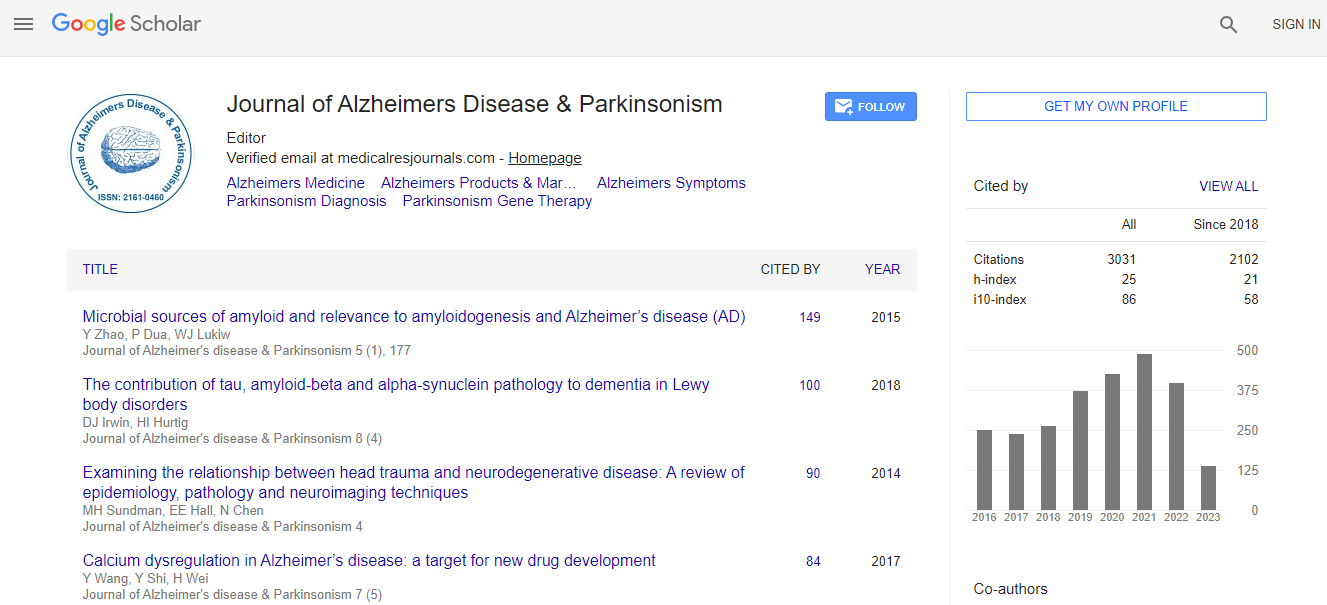
Citation: Brothers HM, Bardou I, Hopp SC, Marchalant Y, Kaercher RM, et al. (2013) Time-Dependent Compensatory Responses to Chronic Neuroinflammation in Hippocampus and Brainstem: The Potential Role of Glutamate Neurotransmission. J Alzheimers Dis Parkinsonism 3:110. doi:10.4172/2161-0460.1000110
Copyright: © 2013 Brothers HM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Chronic neuroinflammation is characteristic of neurodegenerative diseases and is present during very early stages, yet significant pathology and behavioral deficits do not manifest until advanced age. We investigated the consequences of experimentally-induced chronic neuroinflammation within the hippocampus and brainstem of young (4 mo) F-344 rats. Lipopolysaccharide (LPS) was infused continuously into the IVth ventricle for 2, 4 or 8 weeks. The number of MHC II immunoreactive microglia in the brain continued to increase throughout the infusion period. In contrast, performance in the Morris water maze was impaired after 4 weeks but recovered by 8 weeks. Likewise, a transient loss of tyrosine hydroxylase immunoreactivity in the substantia nigra and locus coeruleus was observed after 2 weeks, but returned to control levels by 4 weeks of continuous LPS infusion. These data suggest that direct activation of microglia is sufficient to drive, but not sustain, spatial memory impairment and a decrease
in hydroxylase production in young rats. Our previous studies suggest that chronic neuroinflammation elevates extracellular glutamate and that this elevation underlies the spatial memory impairment. In the current study, increased levels of GLT1 and SNAP25 in the hippocampus corresponded with the resolution of performance deficit. Increased expression of SNAP25 is consistent with reduced glutamate release from axonal terminals while increased GLT1 is consistent with enhanced clearance of extracellular glutamate. These data demonstrate the capacity of the brain to compensate for the presence of chronic neuroinflammation, despite continued activation of
microglia, through changes in the regulation of the glutamatergic system.