Research Article
Bioburden vs. Antibiogram of Diabetic Foot Infection
| Janifer Jasmine1Geethalakshmi Sekkizhar2Satyavani Kumpatla1Vijay Viswanathan1* | ||
| 1M.V. Hospital for Diabetes and Prof. M. Viswanathan Diabetes Research Centre [WHO Collaborating Centre for Research, Education and Training in Diabetes], Chennai, Tamil Nadu, India | ||
| 2Stanley Medical College, Chennai, Tamil Nadu, India | ||
| Corresponding Author : | Dr. Vijay Viswanathan, MD, PhD FRCP (London & Glasgow) M.V. Hospital for Diabetes and Prof. M. Viswanathan Diabetes Research Centre [WHO Collaborating Centre for Research, Education and Training in Diabetes] No:4, Main Road, Royapuram, Chennai-600 013, Tamil Nadu, India Tel: 91-44-2595 49 13-15 Fax: 91-44-2595 49 19 E-mail: drvijay@mvdiabetes.com |
|
| Received September 28, 2013; Accepted November 19, 2013; Published November 25, 2013 | ||
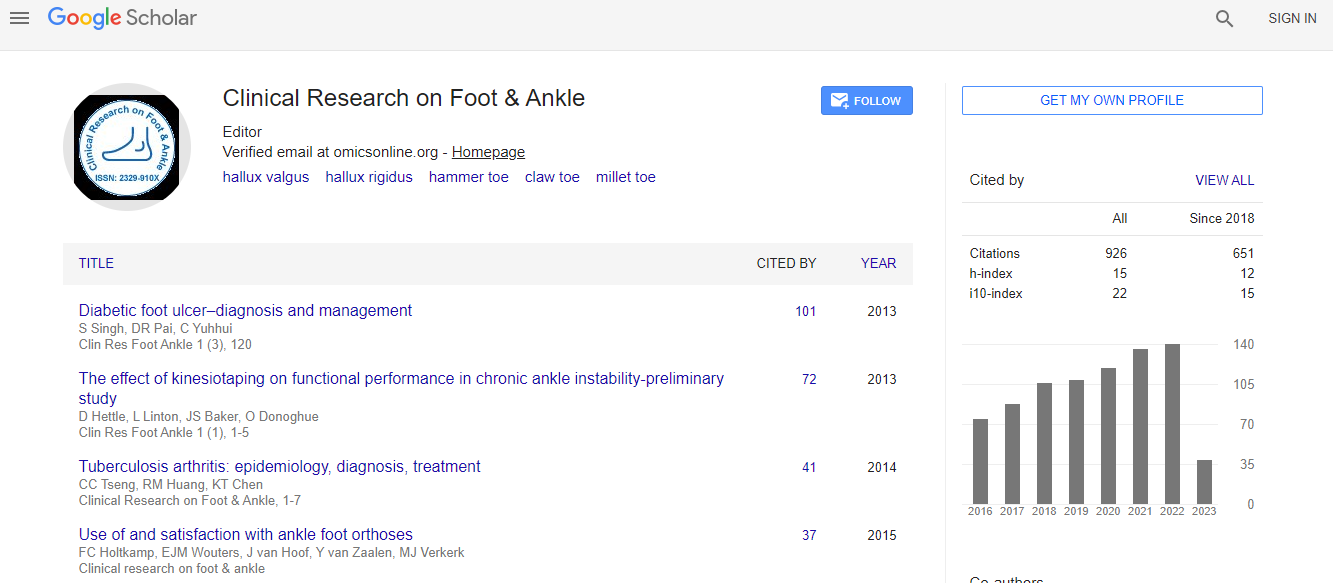
| Citation: Jasmine J, Sekkizhar G, Kumpatla S, Viswanathan V (2013) Bioburden vs. Antibiogram of Diabetic Foot Infection. Clin Res Foot Ankle 1:121. doi: 10.4172/2329-910X.1000121 | ||
| Copyright: © 2013 Jasmine J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. | ||
Related article at  |
||
Abstract
Background: Proper management of diabetic foot infection requires appropriate selection of antimicrobials based on culture and antimicrobial susceptibility testing. The aim was to determine the optimal antimicrobial susceptibility to various commonly used antimicrobials for Gram Positive Cocci (GPCs) and Gram Negative Bacilli (GNBs) in patients with type 2 diabetes and foot infection and also to find out the percentage of MRSA (Methicillin Resistant Staphylococcus aureus) and ESBL (Extended Spectrum of Beta-Lactamase)-producing pathogens and their susceptibility pattern.
Materials and methods: A total of 961 (M: F 697: 264) patients with type 2 diabetes and foot infection were included in this study. After surgical debridement, pus and tissue samples were collected under aseptic conditions in sterile containers and subjected to microbiological analyses. Gram’s staining, culture and sensitivity test were done along with quality control procedures.
Results: Among 961 subjects, single pathogens were isolated in 65.3%, poly-microbial organisms were isolated from 14.3% and 20.4% had sterile cultures. A total of 892 pathogens were isolated, of which 41.1% were GPCs, 57.7% were GNBs and 1.1% were Candida Spp. Imipenem showed the highest sensitivity of more than 95% and Amikacin above 70% against both GPCs and GNBs. Beta-lactam/beta-lactamase inhibitors showed more than 60% sensitivity to GNBs. GPCs were also >75% susceptible to doxycycline, 99.4% sensitive to vancomycin, 89.1% to linezolid, >55% to clindamycin and erythromycin. 1.35% of MRSA and 3.12% of ESBL were isolated from foot ulcers.
Conclusions: In conclusion, Imipenem was found to be the most potential antimicrobial against both GPCs, and GNBs. Among the combinations, cefipime-tazobactum and cefoperazone-sulbactum was the best choice. Anti-MRSA antimicrobials, linezolid and vancomycin and Anti-ESBLs like Imipenem and meropenem can be given to patients producing MRSA or ESBL.