Research Article
Infections of Charcot Feet: Diagnostics and Treatment
| Illgner U* and Wetz HH | ||
| Clinic for Technical Orthopaedic Surgery and Rehabilitation, University Hospital of Muenster,Muenster, | ||
| Corresponding Author : | Illgner U Reinerskamp 19, 48157 Muenster, Germany Tel: 004917638038346 E-mail: ulrich_illgner@web.de |
|
| Received November 12, 2013; Accepted April 21, 2014; Published April 27, 2014 | ||
| Citation: Illgner U and Wetz HH (2014) Infections of Charcot Feet: Diagnostics and Treatment. Clin Res Foot Ankle S3:008. doi:10.4172/2329-910X.S3-008 | ||
| Copyright: © 2014 Illgner U, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. | ||
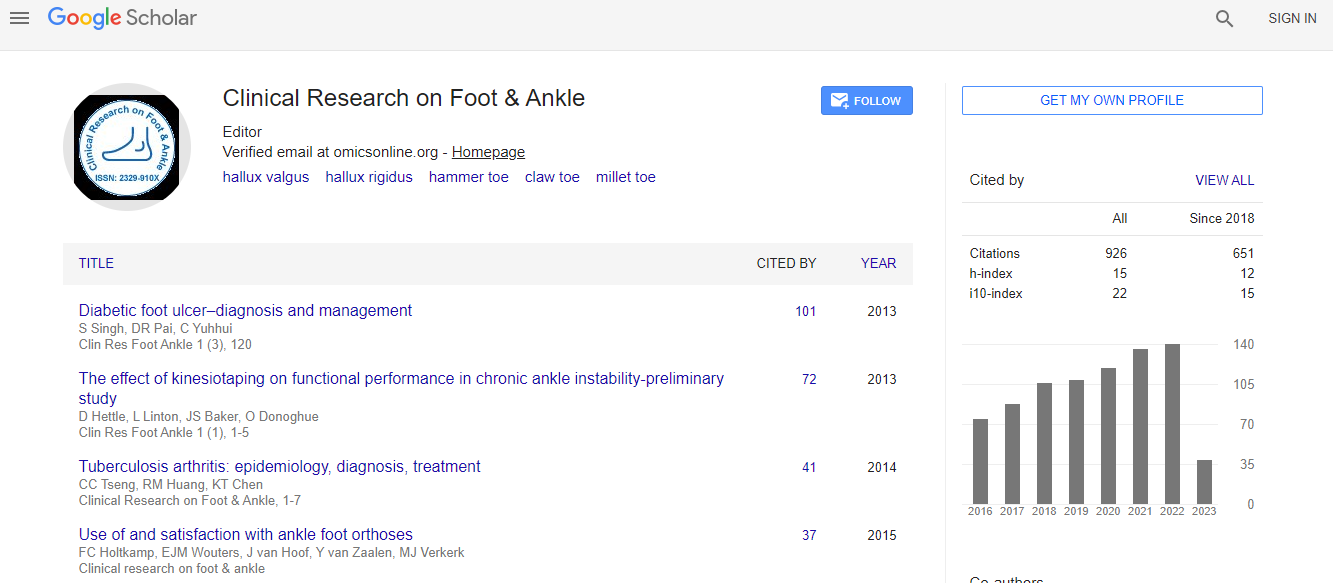
Related article at  |
||
Abstract
Infections of Charcot feet unfortunately remain a common and difficult clinical problem. Because of the polyneuropathy of Charcot feet unrecognized skin lesions and trauma (external pressure) or exostoses (internal pressure) lead to ulceration with consecutive infections. Often these infections are diagnosed too late and still lead too often to amputation. It is essential to examine feet systematically for polyneuropathy and protect feet at risk from infections or detect existing infections as soon as possible. CN itself is a non-infective disease but secondary infections are common. It should be emphasized that any kind of polyneuropathy can cause CN even in the absence of diabetes. Superficial infections and deep infections with osteomyelitis have to be distinguished. If bone can be touched by swabbing osteomyelitis is very likely and represents an indication for surgical intervention in our opinion. Infected bones and soft tissue should be debrided thoroughly; the indication for second look operations should be generous in our opinion, if clinical signs of infections persist after 5-7 days. Amputations should be avoided whenever possible. Antibiotic treatment should be adapted to sensitivity testing of deep samples and maintained for at least 4 weeks. Often there are infections with either multiple germs or complicated bacteria such as MRSA or P.aeruginosa. After surgery the patient needs either protection shoes or, if necessary, customized orthopedic shoes or even orthoses. Side complications as elevated blood glucose level and circulation have to be optimized and the patient has to be informed and trained about his situation. A multidisciplinary team, consisting of orthopaedic surgeon, microbiologist, angiologist, orthopaedic shoe-maker, if necessary diabetologist and rheumatologist is needed.