Risks and Outcomes of Extremity Fractures in Patients with Known Mental Health Disorders: An Ortho-Psychiatric Perspective and a Systematic Review of the Literature
*Corresponding Author: Haroon Majeed, Department of Trauma and Orthopaedic Surgery, Manchester University Foundation Trust, England, United Kingdom, Tel: +44-7766-333650, Email: haroon.majeed@nhs.netReceived Date: May 30, 2020 / Accepted Date: Jun 22, 2020 / Published Date: Jun 29, 2020
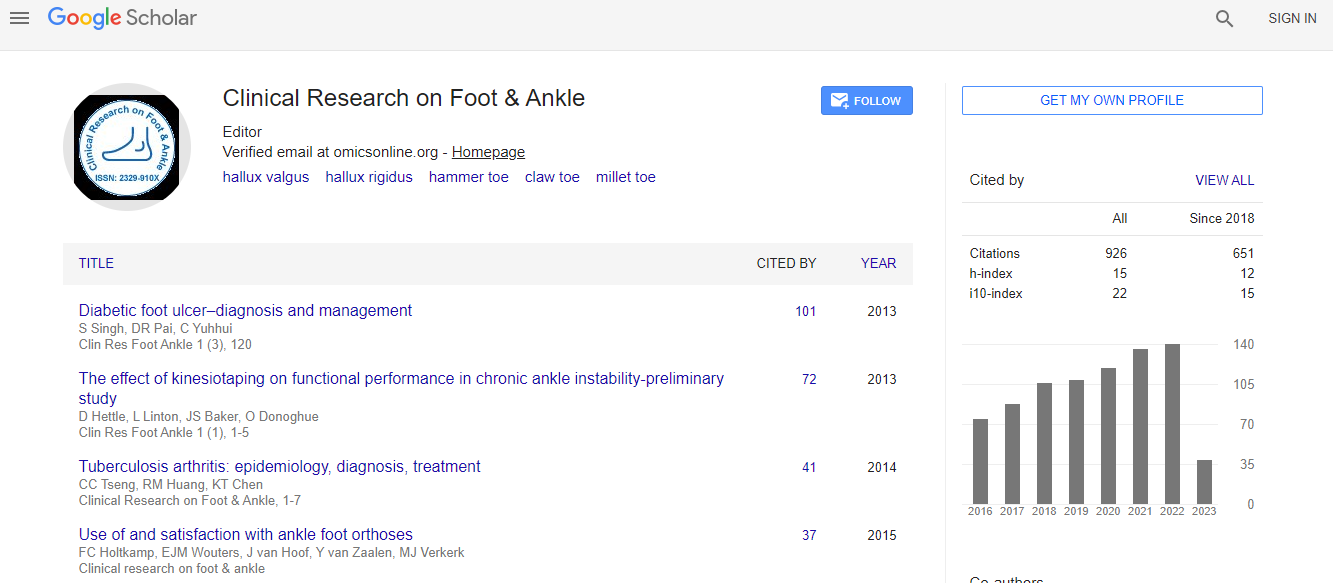
Citation: Saeed U, Majeed H (2020) Risks and Outcomes of Extremity Fractures in Patients with Known Mental Health Disorders: An ‘Ortho-Psychiatric’ Perspective and a Systematic Review of the Literature. Clin Res Foot Ankle 8: 295
Copyright: © 2020 Saeed U, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: We aim to review the risks and outcomes of fractures in patients with pre-existing mental health disorders. Methods: Articles published in the English language from Jan 2000 to March 2020 were searched through PubMed, Ovid, Embase, ScienceDirect and ISI Web of Knowledge. Medical Subject Headings (MeSH) terms were used along with text words. Applying the inclusion and exclusion criteria, of the 390 searched articles, 13 were included for final analysis in line with recommendations from PRISMA guidelines. Main Results: Total participants from all these studies were 1,11,61,087 with a combined mean age of 51.4 years. Two-thirds of the participants were females. The combined mean of fractures and falls was 61.8% among all participants in included studies. The combined mean incidence of mental health disorders was 74.3% among all participants with fractures. Use of psychotropic medications was found to be associated with impairment of cognition, psychomotor function and bone mineral density leading to a substantial increase in fracture risk. Conclusion: Patients with fractures and underlying mental health disorders were reported to have a prolonged hospital stay, poor functional outcomes and increased risk of chronic pain syndrome. Strategies should be in place for early identification of psychiatric disorders following a fracture to mobilize psychosocial support and facilitate discharge.