Our Group organises 3000+ Global Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ ������ Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
������ Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
Citations : 4948
Indexed In
- Index Copernicus
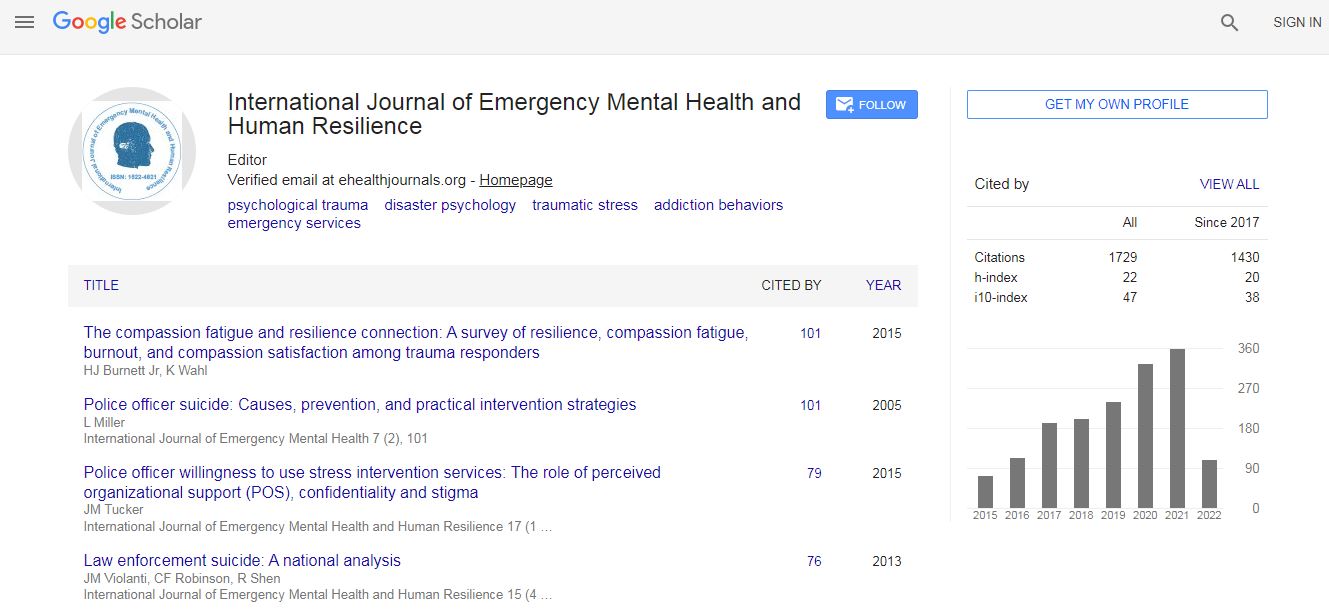
- Google Scholar
- CiteFactor
- Publons
- Pubmed
- science Gate
- scispace
- world cat
Useful Links
Related Subjects
Share This Page
Cognitive disorders and mental health: Neural correlates in contemplative therapy
6th World Congress on Mental Health, Psychiatry and Wellbeing
Denis Larrivee
Loyola University Chicago , USA
Keynote: Int J Emerg Ment Health
Abstract
Writing in 2006, on the occasion of the 100th anniversary of Alloys Alzheimer’s first description of Alzheimer’s Dementia (AD), Dr K Jellinger of the Institute of Clinical Neurobiology, Vienna noted ‘that despite considerable progress in the clinical diagnosis, neuroimaging, genetics, molecular biology, neuropathology, defining risk factors, and treatment, the etiology of the disease is still unknown and, therefore, a causal treatment of AD will not be available in the near future.’ Similar absences mark studies of other notable cognitive diseases, like schizophrenia, suggesting that current models and experimental studies may be directed to non-etiological features of the diseases. Significantly, cognitive diseases display both mental and physical symptomatic signatures. Hence, new conceptions on what is being progressively impaired in these diseases are needed to underwrite therapeutic advances both for the restoration of mental as well as physical health. Such inferences are likely to come from studies on the brain’s global regulation since a key symptom of these diseases is a pathological progression in the loss of self-perception. Existing studies reveal, for example, that a fundamental brain network needed for the self construct, the default mode network (DMN), which is critical to monitoring the external environment, bodily states, and even emotions, is impaired in AD. Furthermore, functional MRI shows that activity in the posterior cingulate and right inferior temporal cortex and that in the bilateral inferior parietal cortex, are differentially affected, reflecting a weakening of causally influential relations amongst the DMN principal nuclei. Schizophrenia patients, on the other hand, display an inability to identify selfinitiated actions, which is likely due to a failure to link self-representations to the body, that may originate in the DMN and premotor cortices. Therapeutic strategies that enhance the neural underpinning of selfrepresentation may, therefore, delay symptomatic progression in these diseases. Increasing evidence suggests that practices that enhance self-integration, like contemplation, may assist in strengthening these features. This talk will discuss current research on the impact of these cognitive diseases on the neural representation of the self, and the potential use of the contemplative practice in strengthening the selfrepresentation and delaying the symptomatic onset.Biography
Denis Larrivee is a Visiting Scholar at the Mind and Brain Institute, University of Navarra Medical School and Loyola University Chicago and has held professorships at the Weill Cornell University Medical College, NYC, and Purdue University, Indiana. A former fellow at Yale University’s Medical School he received the Association for Research in Vision and Ophthalmology’s first place award for studies on photoreceptor degenerative and developmental mechanisms. He is the editor of a recently released text on Brain-Computer Interfacing with InTech Publishing and an editorial board member of the journals Annals of Neurology and Neurological Sciences (USA) and EC Neurology (UK). An International Neuroethics Society Expert he is the author of more than 70 papers and book chapters in such varied journals/venues as Neurology and Neurological Sciences (USA), EC Neurology (UK), Journal of Neuroscience, Journal of Religion and Mental Health, and IEEE Explore. In 2018 he was a finalist in the international Joseph Ratzinger Expanded Reason award.
E-mail: sallar1@aol.com