Our Group organises 3000+ Global Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ 黑料网 Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
黑料网 Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
Citations : 4948
Indexed In
- Index Copernicus
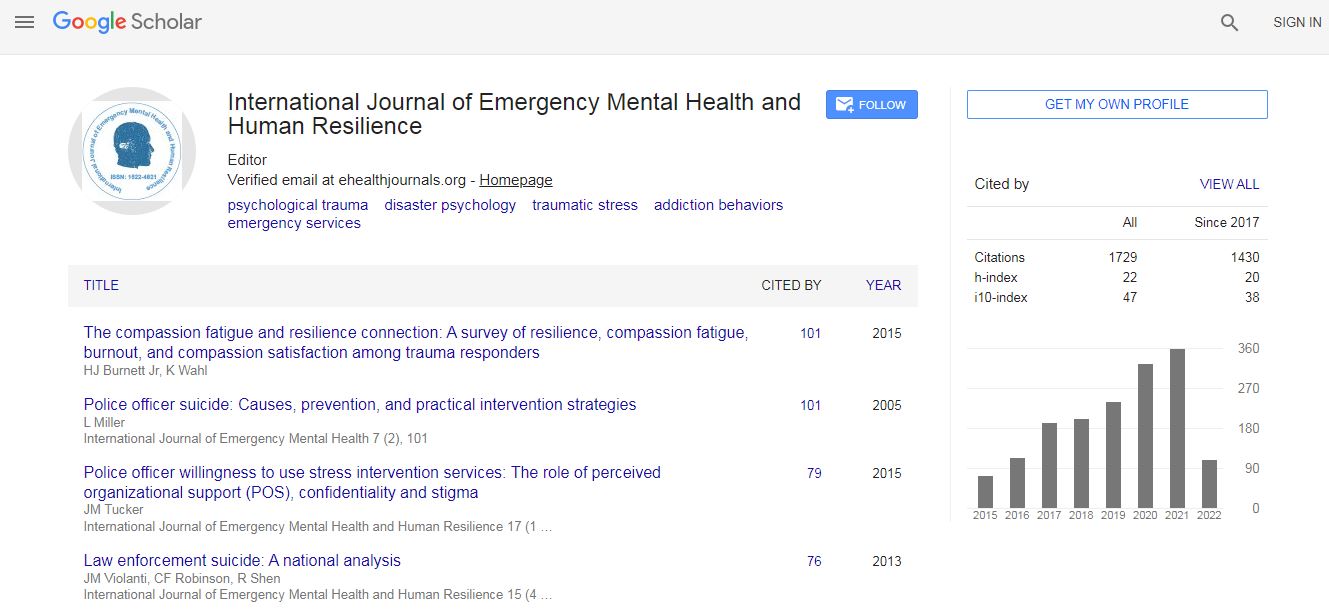
- Google Scholar
- CiteFactor
- Publons
- Pubmed
- science Gate
- scispace
- world cat
Useful Links
Related Subjects
Share This Page
Promoting resilience in families with children with congenital heart disease
5th International Conference on Mental Health and Human Resilience
Gabriella Arrien
William James College, USA
Posters & Accepted Abstracts: Int J Emerg Ment Health
DOI:
Abstract
Congenital heart disease (CHD) is the most common birth defect, affecting approximately 40,000 infants annually in the US. CHD involves a variety of heart defects, with a wide spectrum from simple to moderate to complex. Due to advances in pediatric cardiology and cardiac surgery, life expectancy in these children has increased drastically over the past decades. Now 90% of infants diagnosed with CHD live well into adulthood. Due to the increase in survival rates, attention has shifted towards the impact of CHD on psychological and cognitive functioning. Children with CHD are at risk for neurodevelopmental and psychosocial problems related to operative factors. Children with CHD display lower cognitive functioning, and higher rates in behavioral, attentional and emotional problems. Increased parental stress also adds to the psychosocial issues experienced by these children. For this reason, psychological care is needed to promote resiliency in this population. Incorporating psychological services into treatment protocols with children with CHD is beneficial and will improve behavioral and emotional functioning across their lifespan. This paper will review the definitions of resiliency and Congenital Heart Disease, as well as the professional roles of people treating infants with CHD, the risk factors deterring resiliency, and the developmental outcomes in children with CHD. It will then examine some of the most common psychological interventions for children with CHD and chronic illness, including CBT and psychoeducational interventions, and family-based interventions that also include a psychoeducational component. Author will conclude by discussing the value of this multidimensional approach and why it is the most effective intervention strategy to promote resiliency in children with CHD.Biography
E-mail: garrien31@gmail.com