Research Article
Outcomes and Complications after Biliopancreatic Diversion Based on Age
| Iswanto Sucandy* and Gintaras Antanavicius | |
| Department of Surgery, Abington Memorial Hospital, Abington, Pennsylvania, USA | |
| Corresponding Author : | Iswanto Sucandy, M.D Department of Surgery Abington Memorial Hospital 1200 Old York Road, Abington Pennsylvania 19001, USA Tel: 215-481-7460 Fax: 215-481-2159 E-mail: isucandy@amh.org |
| Received May 13, 2013; Accepted July 10, 2013; Published July 12, 2013 | |
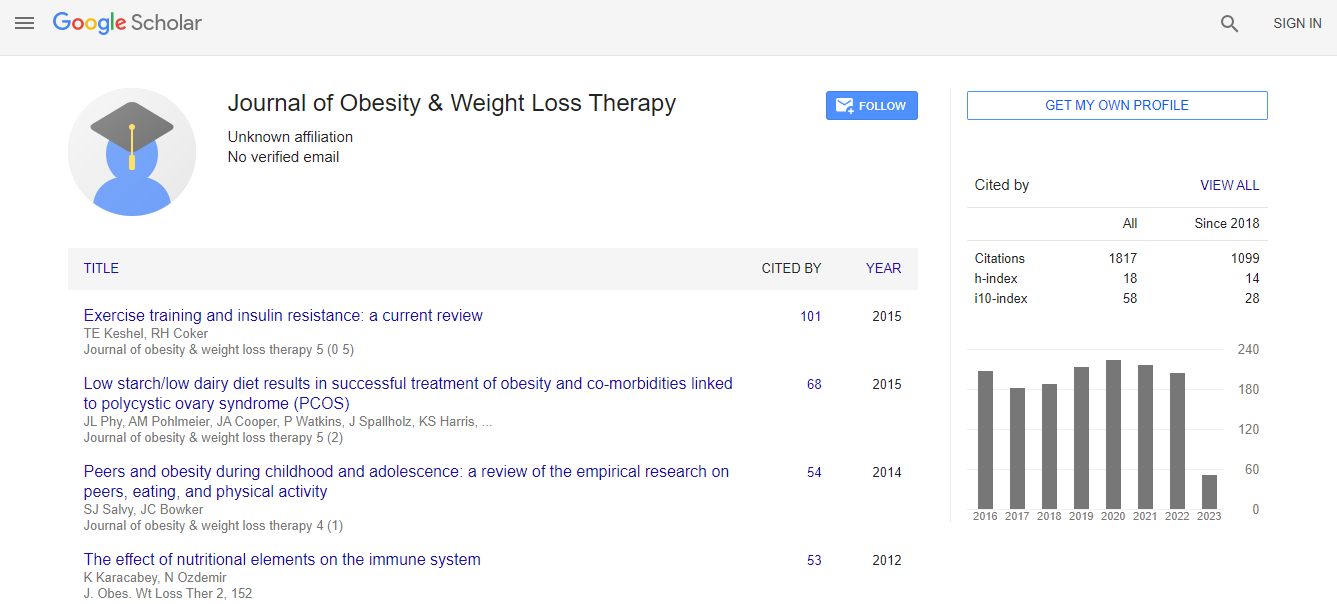
| Citation: Sucandy I, Antanavicius G (2013) Outcomes and Complications after Biliopancreatic Diversion Based on Age. J Obes Weight Loss Ther 3:180. doi:10.4172/2165-7904.1000180 | |
| Copyright: © 2013 Sucandy I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. | |
Abstract
Objectives: Although many risk factors affecting outcomes have been identified, the effect of age on weight loss and perioperative complications was not adequately investigated. Advanced age has been reported to be independently associated with increased complications and inferior weight loss outcome. This study was designed to compare the perioperative complications, and weight loss result after biliopancreatic diversion based on age. Methods: Data of all patients who underwent robotically-assisted laparoscopic biliopancreatic diversion between 2008 and 2011 were reviewed. The patients were divided into the following three age groups for comparison: age 20- 35 years (group A), age 36-50 years (group B), and age 51-72 years (group C). Results: A total of 107 patients were included, with no significant differences in gender, and preoperative BMI among the groups. The oldest group (C) had a statistically significant higher number of preoperative comorbidities, compared with those in groups A and B. No statistically significant differences were found in the mean operative-time or length of stay. There were no intraoperative or 30-day major complications. Percentage of excess weight loss at 1,3,6,9,12, and 18 months postoperatively are comparable among groups. No mortality occurred in this series. Conclusions: Despite a higher number of preoperative comorbidities, older patients perform as well as their younger counterparts with respect to perioperative complications and weight loss outcome.