Our Group organises 3000+ Global Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ ������ Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
������ Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
Citations : 2975
Indexed In
- Index Copernicus
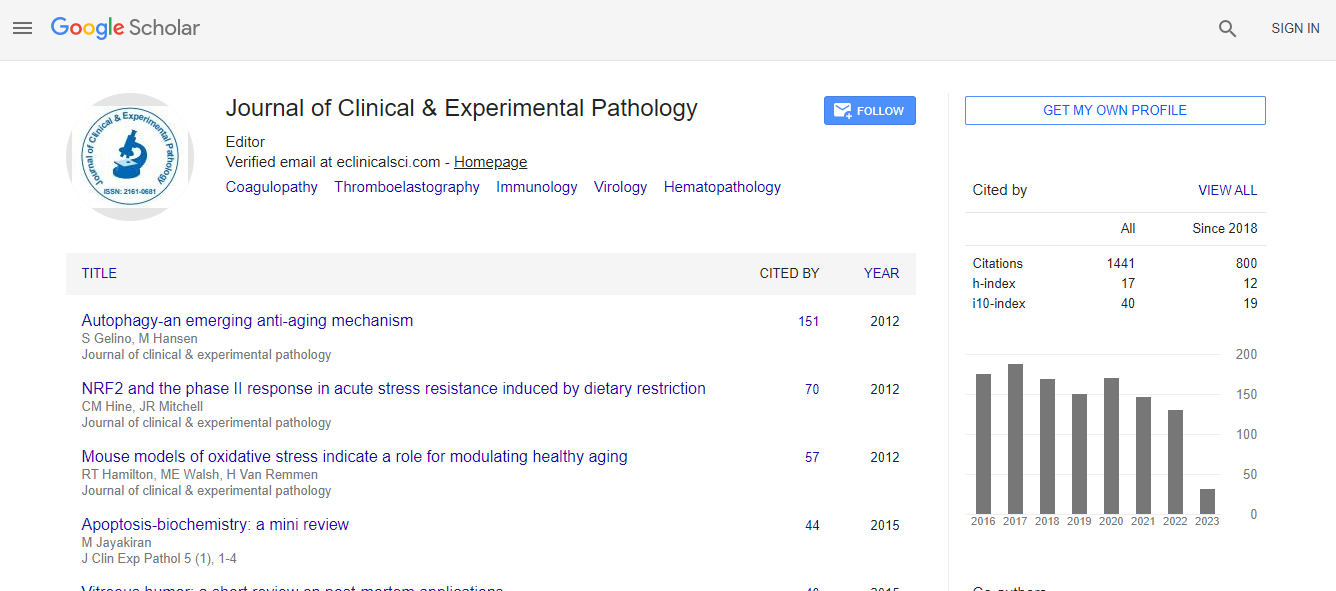
- Google Scholar
- Sherpa Romeo
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Cosmos IF
- Ulrich's Periodicals Directory
- RefSeek
- Directory of Research Journal Indexing (DRJI)
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
- world cat
- journal seek genamics
- j-gate
- esji (eurasian scientific journal index)
Useful Links
Recommended Journals
Related Subjects
Share This Page
Differential adverse events of TNF blockers versus IL-17 axis blockers in treatment of spondyloarthritis
6th European Pathology Congress
Marina N Magrey
Case Western Reserve University, USA
ScientificTracks Abstracts: J Clin Exp Pathol
DOI:
Abstract
Availability of biologics, particularly tumor necrosis factor alpha (TNF-�?±) inhibitors, has revolutionized the treatment of spondyloarthritis (SpA). The main side effect associated with TNF-�?± inhibitors is increased rate of infection. Despite significant concerns about tolerability and adverse events of TNF-�?± inhibitors in treatment of SpA, they have stood the test of time with acceptable safety outcomes. However, there is a subset of patients with psoriatic arthritis (PsA) and ankylosing spondylitis (AS) who fail to respond to TNF-�?± inhibitors, lose efficacy over a period of time, or develop serious adverse events, particularly opportunistic infections. Newer therapeutic options have become available for these patients including interleukin-17 (IL-17) axis antagonists. Their safety data is limited to clinical trials only, with no registry data available as yet. There are no large head-to-head comparative trials between TNF-�?± inhibitors and IL-17 axis inhibitors. Based on data from clinical trials of relatively limited duration, infection rates are quite similar between these two classes of biologics but there are, as yet, no reports of reactivation of opportunistic infections like tuberculosis with IL-17 axis antagonists. However, pre-screening for tuberculosis and prophylaxis in appropriate candidates is still needed. The current available data have shown no other major discrepancies in the adverse events between TNF-�?± inhibitors and IL-17 axis inhibitors. More data is needed to effectively determine the comparative safety of TNF-�?± inhibitors versus IL-17 axis antagonists.Biography
Email: mmagrey@metrohealth.org