Our Group organises 3000+ Global Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ ������ Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
������ Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
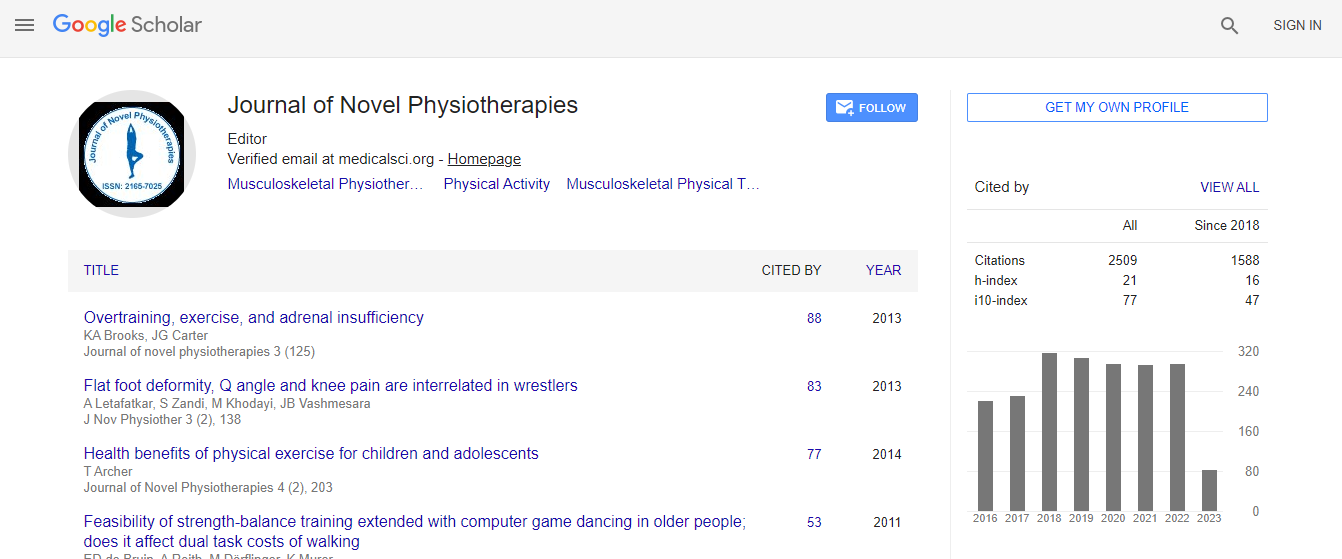
Citations : 3145
Indexed In
- Index Copernicus
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Transcranial direct current stimulation (tDCS) for neurorehabilitation
6th International Conference on Physiotherapy
Areerat Suputtitada
Chulalongkorn University, ThailandKing Chulalongkorn Memorial Hospital, Thailand
Keynote: J Nov Physiother
DOI:
Abstract
Transcranial Direct Current Stimulation (tDCS) has increasingly purposive treatments for neurorehabilitation, compared to other noninvasive neuromodulations. It is inexpensive, safe, easy to administer after well trained, portable, and home used design considered as the most cost effective and good compliance therapy. It can either enhance or suppress cortical excitability by a weak and constant direct current applied to the brain. It has effect for several hours after the stimulation, depending on several factors. Three different stimulation types are as the followings; (1) anodal stimulation, the anodal electrode (+) and the reference electrode are applied over the lesioned brain area and the contralateral orbit, respectively. It effects subthreshold depolarization, producing neural excitation.; (2) cathodal stimulation, the cathode (−) and the reference electrode are applied over the non-lesioned brain area and the contralateral orbit, respectively. It effects subthreshold polarization, suppressing neural activity.; (3) Dual tDCS, anodal and cathodal stimulation, the anodal electrode (+) and the cathodal electrode (−) are applied over the lesioned and non-lesioned brain, respectively. In clinical use, two (or more) electrodes are applied over the scalp with the current flowing from the anodal to the cathodal electrode. The strength of electrical currents cannot produce an action potential. The factors influence neural activity including the state of the brain during stimulation at rest or stimulation and relearning with a task in the meantime, and even the time of the day. There are increasing evidences of tDCS effect on the whole brain networks by stimulating just one brain region. The positive clinical effects of tDCS in various disorders are caused by the complex interactions between the associated brain network and the area of stimulation. Interestingly, stimulation at the dorsolateral prefrontal cortex (DLPFC), have shown the effectiveness for several conditions. On the other hand, different area of stimulation for the same disorder have shown to have similar results. These new evidences may indicate an underlying neural network for disorders and may suggest network stimulation as a new stimulation protocol. Current evidences do not recommend Level A (definite efficacy) for any indication. Level B recommendation (probable efficacy) is revealed for: (i) anodal electrode applied at the left primary motor cortex (M1) and cathodal electrode applied at the right orbitofrontal area in fibromyalgia; (ii) anodal electrode applied at the left dorsolateral prefrontal cortex (DLPFC) and cathodal electrode applied at the right orbitofrontal area in major depressive episode without drug resistance; (iii) anodal and cathodal electrode applied at the right and left DLPFC, respectively in addiction/craving. Level C recommendation (possible efficacy) is revealed for anodal electrode applied at the left M1 or contralateral to pain side and cathodal electrode applied at the right orbitofrontal area in chronic lower limb neuropathic pain secondary to spinal cord lesion. However, Level B recommendation (probable inefficacy) is extended to the absence of clinical effects of: (i) anodal electrode applied at the left temporal cortex and cathodal electrode applied at the right orbitofrontal area in tinnitus; (ii) anodal electrode applied at the left DLPFC and cathodal electrode applied at the right orbitofrontal area in drug-resistant major depressive episode. Whether there is a potential effect when combining tDCS, with intensive physical therapy, constraint- induced therapy, robot-therapy, EMG-triggered functional neuromuscular stimulation is increasing evidences. The evidences revealed combining approaches enhancing adaptive plasticity and limiting maladaptive plasticity according to the stage of the disease, pharmacological, electrophysiological or physical adjuvant therapy could theoretically improve the patients’ care, and given the disease complexity, should ultimately favor a patient-tailored approach. In conclusion, Non-invasive stimulation technique as tDCS have the potential to modulate brain cortical excitability with long lasting effects which promising enhance neurorehabilitation. More researches are upcoming in various indications and stimulation protocols.Biography
Areerat Suputtitada is a Professor of Rehabilitation Medicine, full time working Faculty at Chulalongkorn University and King Chulalongkorn Memorial Hospital in Bangkok, Advisor of the Editorial Board of Thai Rehabilitation Medicine Journal, and an Educational Board Member of Exercise and Health Promotion in the Ministry of Public health. She has published more than 20 international and 30 national articles in the areas of her experts including neurological rehabilitation, spasticity and dystonia, gait and motion and pain.
E-mail: prof.areerat@gmail.com