Our Group organises 3000+ Global Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ ������ Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
������ Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
Citations : 2975
Indexed In
- Index Copernicus
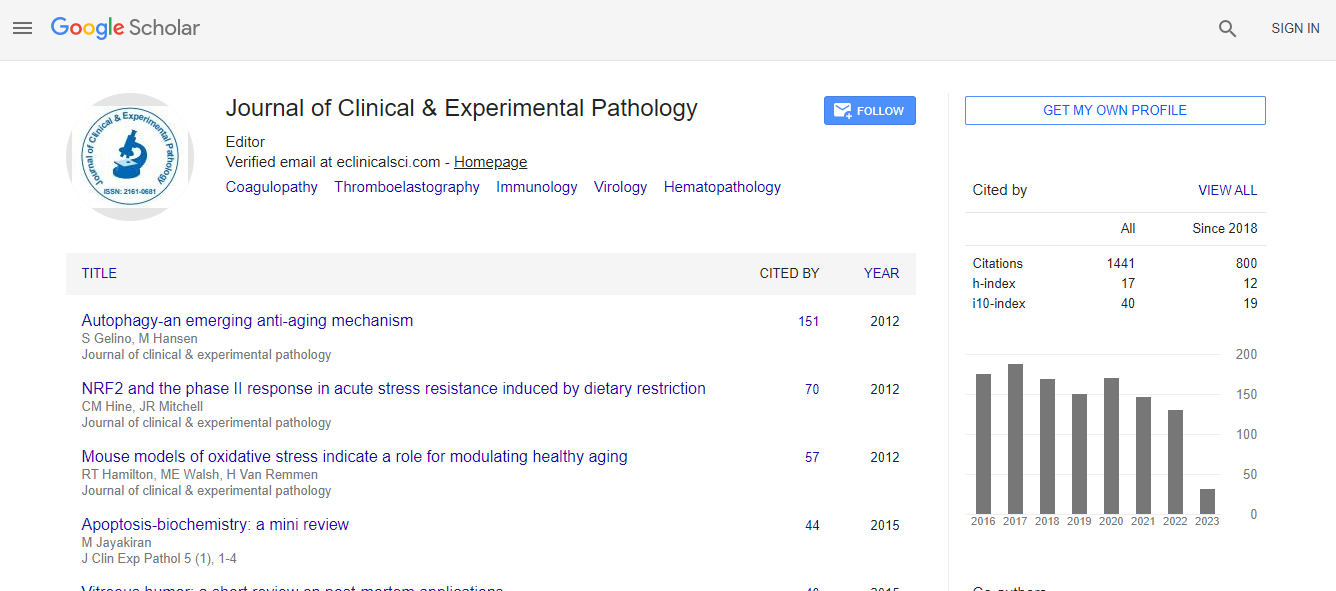
- Google Scholar
- Sherpa Romeo
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Cosmos IF
- Ulrich's Periodicals Directory
- RefSeek
- Directory of Research Journal Indexing (DRJI)
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
- world cat
- journal seek genamics
- j-gate
- esji (eurasian scientific journal index)
Useful Links
Recommended Journals
Related Subjects
Share This Page
Venous thromboembolism in thoracic surgery patients: An on-going challenge
6th European Pathology Congress
Yaron Shargall
McMaster University, Canada
ScientificTracks Abstracts: J Clin Exp Pathol
DOI:
Abstract
Venous Thromboembolism (VTE) is a common postoperative complication resulting in significant morbidity and mortality. Current practice indicates prophylaxis with Low molecular weight (LMWH) or unfractionated heparin during hospital stay. VTE in thoracic surgery is an on-going challenge for surgeons and clinicians looking after those patients. There is a growing evidence that the incidence of VTE events around and after thoracic surgery in significant. It is increasingly recognized that such an event might have a substantial detrimental impact. Yet, high level evidence is, at best, sparse. We have conducted a Delphi protocol survey amongst Canadian surgeons, hematologists and thoracic anesthesiologist which showed that VTE prophylaxis practice is diverse and that there is little agreement within clinicians regarding initiation of treatment, type of prophylaxis and duration. In an additional study, we performed a multicenter prospective cohort study where 157 thoracic oncology patients undergoing resection underwent postoperative assessment with CT PE protocol and venous Doppler to evaluate the real incidence of VTE. All patients received guidelines based pharmaceutical and mechanical prophylaxis until hospital discharge. Patients underwent chest CT angiography with PE protocol and bilateral lower extremity venous Doppler ultrasonography at 30�?±5 days after surgery. VTE incidence was 12.1% (19 VTE events) including 14 PE (8.9%), 3 DVT (1.9%), one combined PE/DVT and one massive left atrial thrombus. Only 4 patients (21.1%) were symptomatic at diagnosis. The 30-day mortality of patients with VTE events was 5.2%. Univariate analysis did not demonstrate significant differences between the VTE and non-VTE populations with regards to baseline and surgical characteristics. We are currently conducting a multicenter randomized control trial comparing post discharge extended prophylaxis with LMWH vs. Placebo, the results of which has the potential to influence and change current practice of in-hospital only VTE prophylaxis. An additional Canadian multi center prospective longitudinal cohort study is undergoing to evaluate the real incidence of VTE events in patients undergoing esophageal resection for cancer. The results of this study will help to support future research into the role of extended prophylaxis in the very high risk population.Biography
Yaron Shargall has completed his Medical school and Bachelor in Medical Sciences and Immunology at the Hebrew University in Jerusalem. Since 2004 he practiced thoracic surgery at the University of Toronto, St. Joseph’s Health Centre and St. Michael’s Hospital. He is currently chairing the European Society of Thoracic Surgeons’ working group on VTE in Thoracic Surgery.
Email: shargal@mcmaster.ca