Our Group organises 3000+ Global Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ ������ Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
������ Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
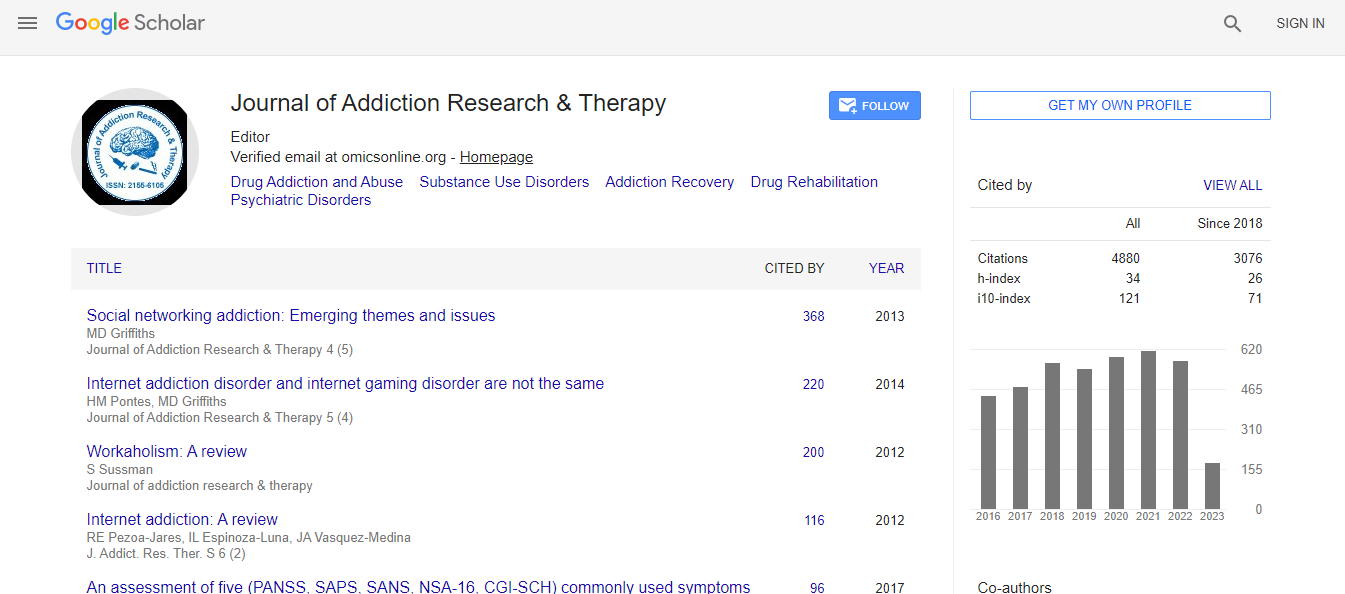
Citations : 4859
Indexed In
- CAS Source Index (CASSI)
- Index Copernicus
- Google Scholar
- Sherpa Romeo
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- SafetyLit
- China National Knowledge Infrastructure (CNKI)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
A retrospective study of retention of opioid-dependent adults in an outpatient buprenorphine/naloxone clinic
8th International Conference on Addiction Psychiatry
David W Hartman and Cheryl W Hartman
Carilion Clinic, USA
ScientificTracks Abstracts: J Addict Res Ther
DOI:
Abstract
Statement of Problem: Globally in 2010 15.5 million people struggled with an opioid use disorder (OUD). OUD is a chronic, relapsing condition leading to significant morbidity and mortality. Since the advent of buprenorphine/naloxone pharmacotherapy with its US FDA approval in 2002, its use has expanded in the US and abroad. This form of medicationassisted treatment (MAT) has been found to decrease mortality and morbidity. Research on long term outcomes of buprenorphine/naloxone treatment is limited by small numbers and short duration of follow-up, leaving unanswered questions about impact of comorbidities and dosing on retention rates and patient outcomes. Purpose: The purpose of this study was to examine retention rates in an office-based opioid treatment clinic at 18 months, identifying opioid abstinence rates, and comparing dosing among long term completers (remaining 18 months or longer) versus non-completers, who exited <18 months. Methodology: A retrospective study was conducted on 182 patients enrolled in the outpatient MAT clinic from 2009-2014. Completion rate was 48.9%. Findings: Findings indicated no gender differences in completion. Significant age differences were evident (p=0.02) with the mean age of completers = 31 vs. 34.7 years for noncompleters. The only psychiatric co-morbidity that predicted reaching the 18 month target was suicidal ideation, odds ratio = 2.35. Patients having suicidal ideation were significantly (p=.045) more likely to remain in treatment for at least 18 months. Number of comorbid diagnoses did not predict retention. Dose of buprenorphine at point of program exit for non-completers was on average = 12.7 mg versus 17 mg for completers (p=00000002.3). There were four non-completers prescribed 24 mg of buprenorphine versus 23 completers on 24 mg. Completers were more likely to be abstinent from opioids compared to non-completers (p=.0002). Result: Results suggest that buprenorphine dose predicts retention. Implications regarding US policies regarding buprenorphine dosing warrant reconsideration. Recent Publications 1. Degenhardt L, Ferrari A J, Calabria B, et al. (2013) The global epidemiology and contribution of cannabis use and dependence to the global burden of disease: Results from the GBD 2010 study. PLoS One DOI:10.1371/journal.pone.0076635. 2. Bell J, Trinh L, Butler B, Randall D and Rubin G (2009) Comparing retention in treatment and mortality in people after initial entry to methadone and buprenorphine treatment. Addiction 104(7):1193- 1200. 3. Genberg B L, Gillespie M, Schuster C R, et al. (2013) Prevalence and correlates of street-obtained buprenorphine use among current and former injectors in Baltimore, Maryland. Addict Behav. 38(12):2868- 2873. 4. Bascaran M T, Garcia Portilla M P, Bobes Bascaran M T, Saiz P A and Bobes J (2014) Long term outcomes of pharmacological treatments for opioid dependence: does methadone still lead the pack? Br J Clin Pharmacol. 77(2):272-284. 5. Fiellin D A, Schottenfeld R S, Cutter C J, Moore B A, Barry D T and O’Connor P G (2014) Primary care– based buprenorphine taper vs. maintenance therapy for prescription opioid dependence: A randomized clinical trial. JAMA Intern Med. 174(12):1947-1954.Biography
David Hartman completed his medical training at Temple University School of Medicine in Philadelphia, PA; his psychiatric residency at the University of Pennsylvania. He is certified as an Addiction Psychiatrist and in Addiction Medicine and is a DATA 2000 waivered physician, credentialed to prescribe buprenorphine. He has been in psychiatric practice in Roanoke, VA since 1982, currently the section chief of Adult Outpatient Psychiatry with Carilion Clinic and is an Associate Professor with the Virginia Tech Carilion School of Medicine. He has created an office-based opioid treatment program at Carilion Clinic, where he has convened a team of practitioners, counselors, care coordinators, and nurses who provide comprehensive treatment services to OUD patients, along with his general psychiatric practice. Academic responsibilities include training medical students, psychiatry residents, and conducting research and quality improvement studies. His research focus has been on OUD medication-assisted treatment with pregnant women and the general adult population Cheryl Hartman completed her Ph.D. in Educational Psychology at Temple University. She has specialized in grantwriting, research, program development and services administration. Her field has included teen pregnancy and school dropout evidence-based programming, as well as substance use disorder prevention. At Carilion Clinic in Roanoke, VA she currently manages the adolescent addiction treatment program and the office-based opioid treatment program, ensuring evidence-based service practices. Cheryl serves on the faculty of the Virginia Tech Carilion School of Medicine and provides training to medical students and medical residents. She is project director for an SBIRT training grant, an ECHO teleconsultation project focused on OUD treatment expansion to rural/underserved communities, and is working on a replication of a manual-guided approach to group therapy with the OUD patients being served in the outpatient clinic.
E-mail: dwhartman@carilionclinic.org