Our Group organises 3000+ Global Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ ║┌┴¤═° Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
║┌┴¤═° Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
Recommended Conferences
Toronto, Canada
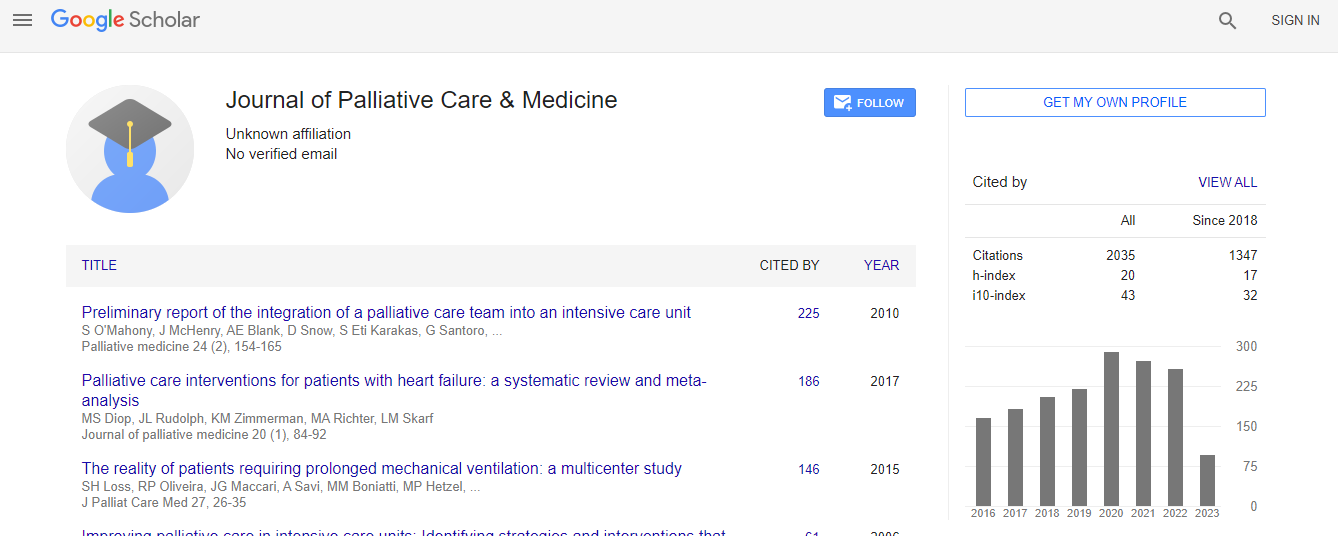
Citations : 2035
Indexed In
- Index Copernicus
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- China National Knowledge Infrastructure (CNKI)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Virtual Library of Biology (vifabio)
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Educational intervention increases primary care providers├ó┬?┬? comfort in discussing advance care planning
International Conference on Hospice & Palliative Care
Margaret Nolan
New York University, USA
Posters-Accepted Abstracts: Posters-Accepted Abstracts
DOI:
Abstract
Background: Advances in medicine have made end-of-life difficult for older adults without prior advance care planning (ACP). Benefits of ACP include decreasing family stress, allowing death with dignity and cost saving at end of life. Despite the benefits, less than a third of the population has ACP. Older adults want their primary care provider to initiate conversations on ACP. Primary care providers rate their own comfort level with ACP discussions as low. The purpose of this project was to increase primary health care providers├ó┬?┬? including physicians, nurse practitioners and physician assistants (PCP) comfort in discussing ACP with their older adult patients. Method: An 8 step educational intervention on best practice for discussing ACP using the Medical Orders for Life Sustaining Treatment (MOLST) Model was conducted in PCP├ó┬?┬?s offices. A convenience sample of 64 primary care providers (PCP) from NYC, who care for patients over 65 years of age, were surveyed using a descriptive, repeated measures design. The pre and posttest instrument is a Communication Strategy Questionnaire for ACP that uses l4-item Likert scale, with scores ranging from 14-56, measuring comfort in discussing ACP. Results: The MOLST intervention significantly improved comfort in discussing ACP for PCP with their patients (p<0.001). Conclusion: A simple 8-step educational intervention demonstrates significant improved comfort level amongst PCPs when discussing end-of-life preferences with patients. Primary care providers can make an impact on older adults├ó┬?┬? end-of-life by discussing advance care.Biography
Email: mn31@nyu.edu