Our Group organises 3000+ Global Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ 黑料网 Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
黑料网 Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
Citations : 739
Indexed In
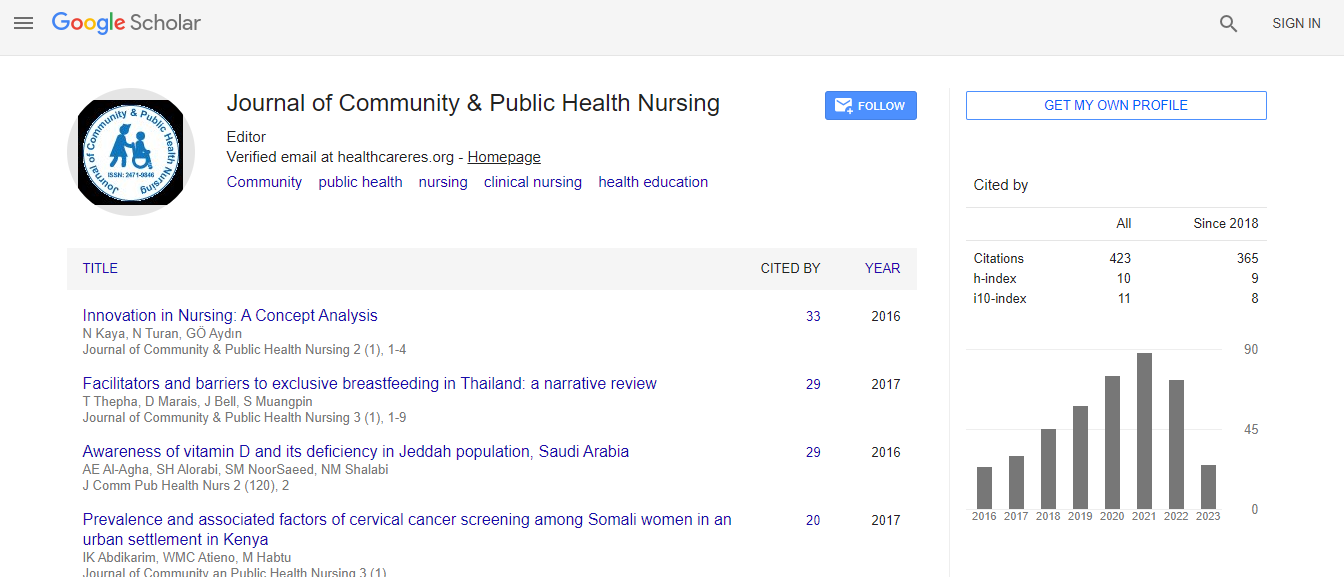
- Google Scholar
- CiteFactor
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Hospital readmission risk screening tools for older adults: A systematic review
25th World Congress on Nursing & Healthcare
Jantra Keawpugdee
Mahidol University, Thailand
Posters & Accepted Abstracts: J Comm Pub Health Nurs
DOI:
Abstract
Background & Aim: Hospital readmissions are defined as multiple inpatient stays within a specified time period by the same patient (Agency for Healthcare Research and Quality, 2013). Screening is the first step in identifying patients at risk for hospital readmissions and predicting readmission to the hospital. The study aims to identify, summarize and evaluate readmission screening tools for older adults. Method: A systematic review of articles written in English and identified via CINAHL, MEDLINE/PubMed, Ovid UML and Cochrane Library was conducted. Additional studies were identified by through reference lists of the identified articles and by Google search. Search items included keywords for readmission, risk assessment, tools and the terms hospital settings and older adults. Reliability, validity and predictors of readmission tools were extracted independently by two authors and categorized by the authors classification tool. Result: 14 studies using five screening tools were identified. Based on the author developed scale screening tools, ISAR, TRST and hospital score showed low to moderate validity and moderate to good reliability. The RRAT validity and reliability scores were low to moderate, and the LACE index validity score was low to moderate, but the reliability of the tool was not reported. Independent variables that were most often identified as predictors of hospital readmission were history of hospital admission, polypharmacy, cognitive and memory problems, the need for help as well as difficulties in walking, the length of stay and comorbid conditions. Conclusion: No single older adult readmission tool stands out as the best hospital readmissions risk screening tool. Tools can be chosen based on ease of use, predictors and hospital needs. Future studies comparing tools with patients with different diagnosis should be conducted.Biography
E-mail: jantrawork@gmail.com