Our Group organises 3000+ Global Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ ������ Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
������ Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
Citations : 739
Indexed In
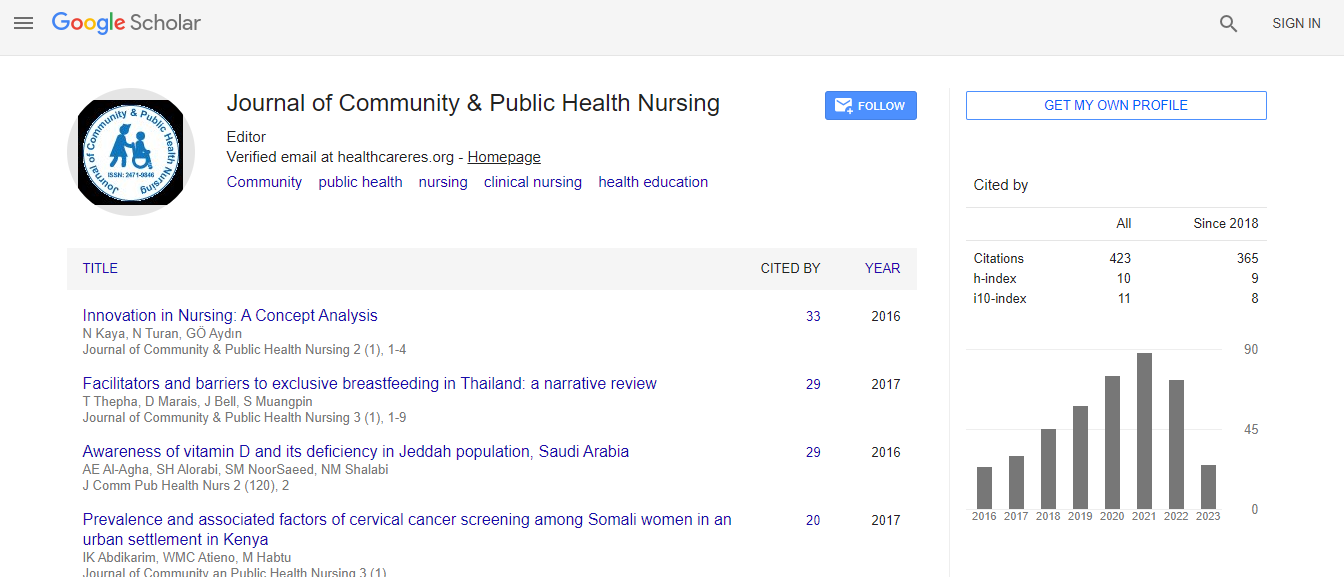
- Google Scholar
- CiteFactor
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
How unified communication improves patient care and safety
7th International Conference on Public Health and Nursing
Asim Masood
William Osler Health System, Canada
Keynote: J Comm Pub Health Nurs
DOI:
Abstract
Hospital communication has become exceedingly complex with multiple and disparate systems. Too often, physiological monitors, beds, IV pumps, ventilators, and other systems sound alarms or send messages to clinical staff that are not actionable. As a result, care team members often suffer from alarm fatigue and become immune sounds and alerts from these systems, which can have serious consequences. In addition, hospitalized patients are also fatigued by the incessant sound of alarms, which often disrupt their sleep and makes them and their family members feel anxious. The impact this noise has on patient, family and staff well-being has accelerated the need to understand alarms, how often they occur, how they are responded to, and how to manage them safely and efficiently. Being able to connect the right people with the right information quickly is critical to delivering safe patient care in a quiet, healing environment. Methodology/Approach: William Osler Health System implemented an intelligent alarm management solution to improve patient care, safety and experience across three sites. With the solution, alerts and alarms are automatically sent to the right care team member(s) based on workflow and escalation rules defined in the system. Clinicians can easily distinguish between alarms from multiple sources and different criticalities based on the audio and visual information sent directly to their device of choice – whether it’s a smartphone, laptop or workstation. The solution enables them to quickly prioritize alarms and respond appropriately. All alarm events and responses are date and time stamped and logged in real time, providing robust data and an audit trail to identify potential gaps in communication and processes. Analytics from the solution helps hospital leaders understand alarm trends per bed, unit, staff, alarm type, alarm density, distribution and response times. This data allows refinement of alarm filtering and escalation to reduce alarm fatigue, improve patient safety and enhance care team efficiency. Findings/Results: Integration of the alarm management solution with clinical systems such as the EHR, nurse call system, and physiological monitors has streamlined workflows and minimized the complexity of managing multiple systems and vendors. One of the most impactful alerts set up connects the communication system to a point-of-care decision-support application. The software monitors patient data gathered from the EHR system, looking for early signs of a developing infection. When the system detects early warning signs of sepsis, it automatically sends an alarm to the appropriate nurse on his or her device of choice. With early warning, hospital staff can act immediately to accelerate treatment and improve patient outcomes. These workflow integrations and intelligent codes have helped decrease code blue events and ICU transfers. Clinicians have also noted a decrease in mortality rates. Conclusion/Recommendations: In integrated approach to communication and alarm management is key to reducing alarm or interruption fatigue, increase staff response times, and improve the healthcare experience. Mobile healthcare technology that is fully integrated to workflows and with clinically relevant patient data can also lead to better patient outcomes.Biography
Masood also held the roles of Deputy Chief of Staff and Chief Medical Information Officer at William Osler Health System (Osler) from 2005 to 2015. In 2015, he was appointed as the Regional Chief Medical Information Officer for Osler, Headwaters Healthcare Centre and the Central West Community Care Access Centre in Brampton and Orangeville, Ontario.
E-mail: hikaramba@gmail.com